Normal
0
false
false
false
EN-US
X-NONE
X-NONE
/* Style Definitions */
table.MsoNormalTable
{mso-style-name:”Table Normal”;
mso-tstyle-rowband-size:0;
mso-tstyle-colband-size:0;
mso-style-noshow:yes;
mso-style-priority:99;
mso-style-qformat:yes;
mso-style-parent:””;
mso-padding-alt:0in 5.4pt 0in 5.4pt;
mso-para-margin-top:0in;
mso-para-margin-right:0in;
mso-para-margin-bottom:10.0pt;
mso-para-margin-left:0in;
line-height:115%;
mso-pagination:widow-orphan;
font-size:11.0pt;
font-family:”Calibri”,”sans-serif”;
mso-ascii-font-family:Calibri;
mso-ascii-theme-font:minor-latin;
mso-hansi-font-family:Calibri;
mso-hansi-theme-font:minor-latin;
mso-bidi-font-family:”Times New Roman”;
mso-bidi-theme-font:minor-bidi;}
Diabetic ulcers, prevalent among individuals with diabetes, present intricate challenges in healthcare due to their chronic nature and increased susceptibility to complications. Addressing these ulcers requires a meticulous and multifaceted approach tailored to the specific needs of patients, aiming to promote healing, prevent infections, and preserve limb function.
Key elements integral to managing diabetic ulcers encompass:
- Early Detection and Assessment: Timely identification and continuous monitoring of diabetic ulcers are crucial. Comprehensive assessments of ulcers, considering factors like neuropathy, vascular status, and wound characteristics, guide treatment decisions.
- Wound Bed Preparation and Debridement: Effective wound bed preparation involves debridement to remove necrotic tissue and create an optimal environment for healing. This step is pivotal in promoting tissue regeneration and reducing infection risks.
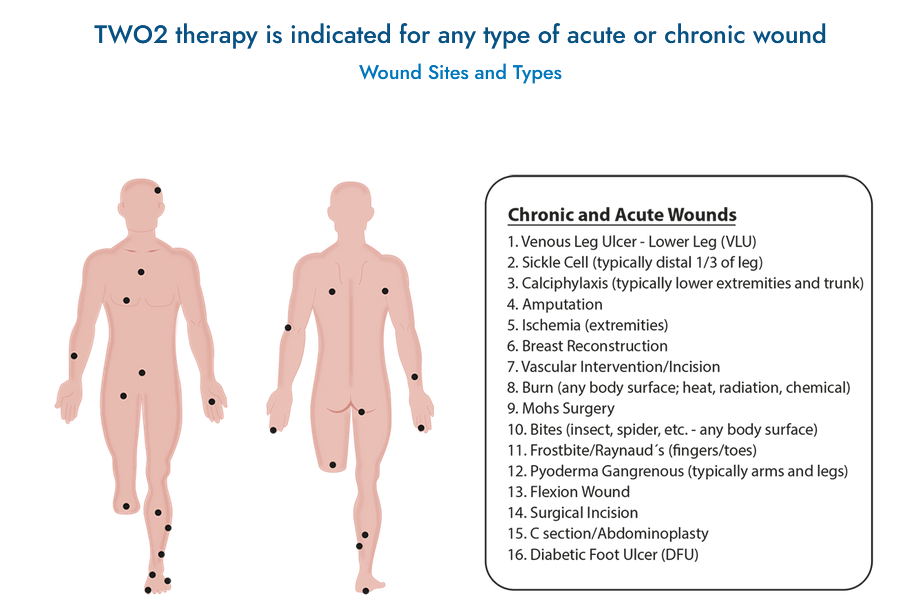
- Specialized Wound Care Treatments: Utilization of advanced therapies such as growth factor treatments, bioengineered skin substitutes, and negative pressure wound therapy (NPWT) can expedite healing and mitigate complications associated with diabetic ulcer.
- Comprehensive Diabetes Management: Integrating wound care with comprehensive diabetes management, including glycemic control, foot care education, and lifestyle modifications, helps address underlying factors contributing to ulcer development.
Collaboration among a multidisciplinary team comprising podiatrists, wound care specialists, endocrinologists, nurses, and vascular surgeons is vital. Their collective expertise ensures a holistic approach, addressing not only the wound but also the systemic factors affecting healing.
Diabetic ulcers often pose challenges beyond physical healing, impacting patients’ daily lives and well-being. Patient education on preventive measures, foot care practices, and early warning signs empowers individuals to actively participate in managing their condition.
Investments in research and innovations in diabetic ulcer care reflect a commitment to improving patient outcomes and reducing the burden of these chronic wounds. Ongoing advancements aim to enhance treatment efficacy, reduce healing times, and prevent severe complications.