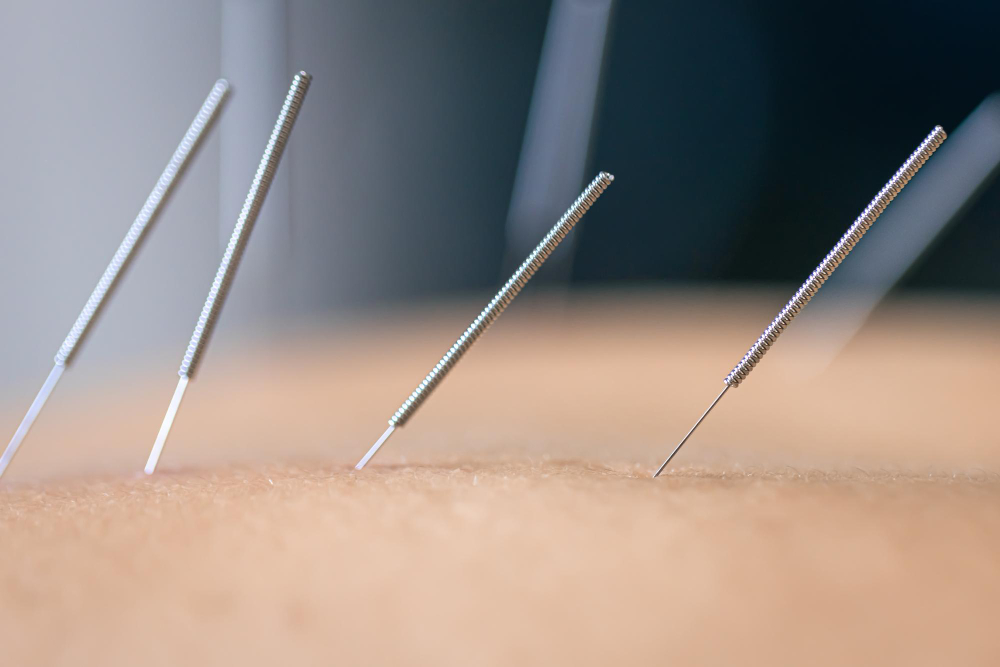
Needlestick injuries (NSIs) are a serious occupational hazard for health care workers (HCWs) who are exposed to bloodborne pathogens such as HIV, hepatitis B and C, and other infections. NSIs can cause physical, psychological, and financial harm to the affected HCWs and their families, as well as increase the risk of transmission of infections to patients and the community. According to the World Health Organization (WHO), more than 3 million HCWs suffer from NSIs each year.
The prevention of NSIs is a priority for health care organizations and policy makers, as it can save lives, reduce morbidity and mortality, and decrease the costs associated with testing, treatment, and compensation. The WHO recommends a comprehensive approach to NSI prevention that includes the following elements:
● Establishing a safe work environment that minimizes the risk of exposure to blood and body fluids
● Providing adequate training and education on infection prevention and control practices, including the correct use and disposal of sharps
● Implementing standard precautions for all patients and procedures, regardless of their infection status
● Using safety-engineered devices (SEDs) that have built-in features to prevent or reduce the risk of NSIs, such as retractable needles, needleless systems, or blunt suture needles
● Reporting and recording all NSIs and exposures to blood and body fluids, and providing post-exposure prophylaxis (PEP) and follow-up care as needed
● Monitoring and evaluating the effectiveness of NSI prevention interventions and policies
By following these recommendations, health care organizations can create a culture of safety that protects HCWs from NSIs and improves patient outcomes. NSI prevention is not only a moral obligation, but also a legal and ethical responsibility for health care leaders, managers, and workers. Together, we can reduce the risk of NSIs and make health care safer for everyone.
NEEDLESTICK INJURY PREVENTION AMONG HEALTHCARE WORKERS
Needlestick injuries are a serious occupational hazard for healthcare workers, especially those who handle blood or other potentially infectious materials.
Needlestick injuries are preventable, but they require a comprehensive approach that involves engineering controls, work practices, personal protective equipment, education and training, and post-exposure management. In this blog post, we will discuss some of the best practices for preventing needlestick injuries among healthcare workers.
Engineering controls are the primary means of preventing needlestick injuries. They involve the use of devices that reduce or eliminate the risk of exposure to blood or other potentially infectious materials. Examples of engineering controls include:
● Safety-engineered needles and syringes that have built-in features to prevent accidental needlesticks, such as retractable needles, shielding mechanisms, or blunting tips.
● Needleless systems that avoid the use of needles altogether, such as intravenous catheters, connectors, and valves that allow for the administration of fluids and medications without piercing the skin.
● Sharps containers that are puncture-resistant, leak-proof, and clearly labeled to safely dispose of used needles and other sharps.
Work practices are the behaviors and actions that healthcare workers perform to reduce the risk of exposure to blood or other potentially infectious materials. Examples of work practices include:
● Following standard precautions for infection prevention and control, such as washing hands before and after patient contact, wearing gloves and other appropriate personal protective equipment, and avoiding contact with blood or body fluids.
● Using safety-engine standard precautions for infection prevention and control, such as washing hands before and after patient contact, wearing gloves and other appropriate personal protective equipment, and avoiding contact with blood or body fluids.
● Using safety-engineered needles and syringes correctly and consistently, according to the manufacturer’s instructions and institutional policies.
● Never recapping, bending, breaking, or manipulating used needles in any way that could cause injury or exposure.
● Disposing of used needles and other sharps immediately after use in a designated sharps container that is close to the point of use.
● Reporting any needlestick injury or exposure incident to the supervisor or occupational health service as soon as possible.
Personal protective equipment (PPE) is the last line of defense against needlestick injuries. It consists of specialized clothing or equipment that healthcare workers wear to protect themselves from exposure to blood or other potentially infectious materials. Examples of PPE include:
● Gloves that are appropriate for the task and fit well. Gloves should be changed between patients and whenever they are torn or contaminated.
● Gowns, aprons, or lab coats that cover the arms and body to prevent contact with blood or body fluids.
● Masks, goggles, face shields, or other eye protection that prevent splashes or droplets from reaching the eyes, nose, or mouth.
● Shoe covers or boots that protect the feet from exposure to blood or body fluids.
Education and training are essential for raising awareness and promoting compliance with needlestick injury prevention measures. Healthcare workers should receive regular education and training on:
● The risks and consequences of needlestick injuries and exposure to bloodborne pathogens.
● The availability and use of safety-engineered devices and needleless systems.
● The proper work practices and procedures for handling needles and other sharps.
● The correct use and disposal of personal protective equipment.
● The post-exposure management protocol and resources.
Post-exposure management is the process of providing appropriate care and support to healthcare workers who experience a needlestick injury or exposure incident. Post-exposure management should include:
● Prompt wound care, such as washing the affected area with soap and water, applying antiseptic, and covering with a sterile dressing.
● Immediate medical evaluation by a qualified health professional who can assess the risk of infection and provide counseling, testing, prophylaxis, treatment, follow-up, and referral as needed.
● Psychological support to address any emotional distress or anxiety caused by the incident.
● Documentation and investigation of the incident to identify the source patient, determine the type and severity of exposure, evaluate the effectiveness of preventive measures, and recommend corrective actions.
Needlestick injuries are a preventable but serious threat to the health and well-being of healthcare workers. By implementing a comprehensive approach that involves engineering controls, work practices, personal protective equipment, education and training, and post-exposure management, healthcare workers can protect themselves from needlestick injuries and reduce the risk of infection from bloodborne pathogens.